FAQs: Interventional
CT Guided Biopsies
Why might I need a CT scan if I am having a biopsy?
The radiologist performing your biopsy may use a CT scanner to observe and follow the biopsy needle as it approaches and reaches the targeted tissue within your body. CT imaging significantly shortens the amount of time it takes to complete the biopsy and increases the accuracy of your diagnosis.

How should I prepare for a CT scan if I am having a biopsy?
To prepare for a CT scan, we recommend you dress comfortably. Also, avoid any clothing that contains metal objects such as snaps or zippers that can affect the CT image. Depending on your individual scan, you may be asked to drink contrast before you arrive. Contrast material is a dye that makes your organs and blood vessels more visible when you are scanned.
What type of CT equipment is used for guided biopsies?
The CT scanner is a specialized machine that looks like a large doughnut. You will lie on a movable table that goes in and out of the center of the machine. Most CT studies use an advanced unit called a spiral CT that records a large number of pictures in a short time.
Abscess Drainage
What is abscess drainage?

Abscess drainage is a procedure to drain an infection in the body, such as the chest, abdomen, or pelvis, by insertion of a thin tube (catheter) into the abscess to drain the site of the infection. The catheter will drain the abscess from your body.
What does an abscess drainage treat?
An abscess drainage treats abscesses that can be found in various places in your body. Abscesses can impair blood flow to neighboring areas of your body. As a result, these areas are deprived of nutrients which can result in the loss of a limb if an abscess is ignored. Treating your abscess early is very important.
What causes an abscess?
An abscess can start anywhere in the body where bacteria is infecting tissue. A bacterial infection can cause an abscess to form. Abscesses occur more often in patients with inflammatory bowel disease (Crohn’s disease), trauma, surgery, or intestinal perforation. They also can be caused by minor breaks and punctures in the skin, obstruction of sweat glands and oil glands, and inflammation of hair follicles. An abscess contains dead cells, bacteria, and other debris, which causes inflammation and pain. People with weakened immune systems may be more prone to abscesses or may have more severe ones.
What are the symptoms of an abscess?
Symptoms of abscess include:
- Fever
- Chills
- Sweating
- Infection
- Pain
Who is at risk for an abscess?
An abscess may form in an area of the body from different causes. Patients with inflammatory bowel disease (Crohn’s disease), trauma, surgery, or intestinal perforation are at risk for abscesses. Sometimes abscesses occur after a surgery and will delay your recovery. Although antibiotics can help, they cannot really be effective against a large abscess.
Who is a candidate for abscess drainage?
A ultrasound or CT can detect an abscess. You are a candidate for abscess drainage if your physician believes that your abscess can be treated by drainage instead of operation. Very occasionally is an operation required.
What should I expect before my abscess drainage?
First you will have blood drawn and an IV (intravenous catheter) of antibiotics to prevent infection. A CT scan will be done to ad the physician in inserting the tube for drainage.
What happens during my abscess drainage?
During the procedure you will be attached to a monitor so that IV medications can be given to relax you. The skin over your abscess will be cleaned and numbed. The CT scan will next be used in guiding the physician in inserting a tube into the abscess. The tube will be attached to a drainage bag outside of your body. More than one tube may be required depending on the condition of the abscess.
How successful is abscess drainage?
Although there are risks in an abscess draining, it does rid the body of infection so that you can heal quicker from your infection. Usually you will feel better the next day. It will almost certainly result in a great improvement in your medical condition.
What should I expect after the procedure?
You will be admitted to the hospital at least overnight to monitor and treat your pain and observe the amount of drainage from your tube. The nurse will teach you how to care for your tube once you return home. You will then set up a date to return for your follow-up CT scan. The physician will let you know how long you will have your tubes. If needed, a home health nurse can come to your home to help you care for your tube(s). The drainage can be sent to the laboratory for tests to show which is the best antibiotic to treat the remaining infection.
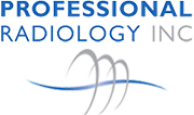
Angioplasty
What is angioplasty?
Angioplasty is a minimally-invasive procedure that repairs and restores blood flow through a narrowed or blocked artery. The procedure is performed by an interventional radiologist.
What is the benefit of having angioplasty?
Angioplasty can prevent a heart attack or stoke by opening your blocked artery, restoring blood flow to your tissues and relieving your symptoms without the need for surgery.
Why do I need angioplasty?
The most common reason for angioplasty is to relieve a blockage of an artery caused by atherosclerosis, or hardening of the arteries. Atherosclerosis is a gradual process in which cholesterol and other fatty substances in the bloodstream form a substance called plaque on the inside of the blood vessel walls and clog the artery. When medications or lifestyle changes aren’t enough to reduce the effects of blockages in your arteries, or if you have worsening chest pain or heart problems your doctor may suggest angioplasty. If you have extremely hard plaque deposits, blockages, or blood vessel spasms that don’t go away, you probably are not a good candidate for angioplasty.
What should I expect before my angioplasty?
Prior to the procedure, you may have several tests performed, such as X-rays and blood tests. You will be asked not to eat or drink anything after midnight the night before your procedure. You should tell the interventional radiologist or nurse if you are allergic to any medications. Angioplasty usually requires an overnight hospital stay. Make sure you arrange for transportation home.
What happens during my angioplasty?
Angioplasty is performed by a specially-trained doctor, called an interventional radiologist.
The interventional radiologist will use an intravenous (IV) line to give you fluids and medicines that will relax you and prevent blood clots. Next the nurse will:
- Shave the area where the catheter or tube will be inserted, usually the arm or groin.
- Clean the shaved area to make it germ free.
- Numb the area.
When you are comfortable, the interventional radiologist will begin the procedure.
- A small incision is made in the skin to find an artery. The doctor then threads a very thin wire through the artery up to the coronary artery that is blocked.
- When the wire reaches the area of the blockage, a tube (called a catheter) with a deflated balloon on the end is threaded into the blocked artery under X-ray guidance.
- A small amount of dye may be injected through the tube into the blood stream to help show the blockage on X-ray. This X-ray picture of the heart is called an angiogram.
- When the tube reaches the blockage, the balloon is inflated. The expanding balloon forces the blockage to open by pushing the walls of the artery outward, increasing blood flow to the heart muscle.
- A stent usually is placed at the site to keep the artery open. Once the balloon has been deflated and withdrawn, the stent remains in place permanently, holding the blood vessel open and restoring blood flow to the arteries.
What should I expect after the procedure?
Your catheter site will be checked for bleeding and swelling after the procedure. Your blood pressure and heart rate will be monitored. Your physician may prescribe medication to relax you and protect your arteries against spasm and to prevent blood clots. Usually you will stay at the hospital overnight and return home the day after the procedure. You typically will be able to walk within two to six hours following the procedure and return to your normal routine by the following week.
For more information about this procedure or general information about our interventional radiology practice, please contact one of our clinical coordinators at 513-527-9999.
Endovenous Laser Ablation of Varicose Veins
What are varicose veins?

Normally, veins in the leg return blood to the heart by the pumping action of the muscles when a person walks. One-way valves prevent reflux of blood back into the legs. Veins become less elastic and the valves can begin to malfunction. When this happens, the veins become distended and take on a ropy appearance that can be unsightly and cause pain, swelling, or itching. Standing and walking may become uncomfortable. Some of the causes of varicose veins are: age, heredity, pregnancy, and weight gain. Endovenous laser ablation may provide a solution to the problem.x
What is endovenous ablation of varicose veins?
Endovenous laser ablation is a less invasive alternative to standard vein stripping for patients suffering from varicose veins. The procedure treats the vein(s) from the inside using heat energy from a laser source to seal the afflicted vein(s). Local anesthesia is all that is required.
Interventional radiologists perform this procedure on an outpatient basis and when compared with traditional surgical techniques, endovenous laser ablation is as effective, has fewer negative outcomes, and is associated with less pain during recovery. There are virtually no scars because catheter placement requires skin openings of only a few millimeters, not large incisions.
What happens during the procedure?
Unlike older, more invasive procedures that strip veins from the leg through the use of small incisions, endovenous laser ablation uses a catheter, or small tube, which is inserted through a small nick in the skin. Only local anesthesia is required.
The leg being treated will be sterilized and covered with a surgical drape. A local anesthetic will be administered to the site where the incision will be made, generally immediately above or below the knee. Let your doctor know if you have an allergy to anesthetics.
The procedure starts by advancing the catheter inside the vein up to the top of the leg. Anesthetic is injected along the vein(s) being treated. Energy is applied as the catheter is slowly withdrawn. This heats and seals the vein closed. By the time the heat energy is delivered, the vein will be numb and there should be no pain. Throughout the procedure, the radiologist guides the catheter using the external ultrasound wand positioned directly outside on the surface of the leg.
How long does the procedure take?
The procedure takes about 45 minutes to one hour right in our vascular clinic.
What happens after the procedure?
A compression stocking must be worn after the procedure to help reduce bruising, tenderness, and the slim possibility of forming blood clots. Normal activity can be resumed, with the exception of lifting heavy objects or prolonged sitting (for instance a long plane or bus trip).
Four weeks after endovenous laser ablation, the radiologist will follow up using ultrasound to ensure that the procedure was successful at treating the vein(s) in the leg. Minor additional procedures to treat associated veins may be necessary.
How long do the effects of treatment last?
In clinical trials, laser treatment has proved to be 97% effective. Therefore, you should experience no recurrence in the veins that have been treated. However, you may want to have follow-up procedures to obtain the best cosmetic results.
How safe is endovenous laser ablation?
Medical lasers work by delivering light energy to the targeted tissue with extreme precision so as not to harm the surrounding tissue. Lasers are proven to be safe and effective for treating many health issues. In the hands of a skilled physician, lasers offer far less risk and complications than conventional surgery.
Endovenous laser ablation is generally a complication-free and safe procedure. Most patients report their symptoms are greatly reduced after the varicose veins are treated.Many patients experience bruising and tenderness after the procedure. Wearing compression stockings and taking anti-inflammatory medication may take away some of the tenderness. In addition, there have been some reports of heat damage to nerves, although this is rare and often goes away over time. Lastly, it is possible for blood clots to form in the leg veins. If this occurs, the clot can travel to the lungs causing a pulmonary embolism. However, this reaction is extremely rare.
Will I need repeat procedures to maintain or improve my results?
Endovenous laser ablation is successful at closing the treated vein(s) nearly 100 percent of the time. Small dilated branches that persist often require additional treatment with phlebectomy (a minor surgical procedure to extract them) or injection of a liquid agent to seal them off, called sclerotherapy. Subsequent treatments can be scheduled two to four weeks after ablation.
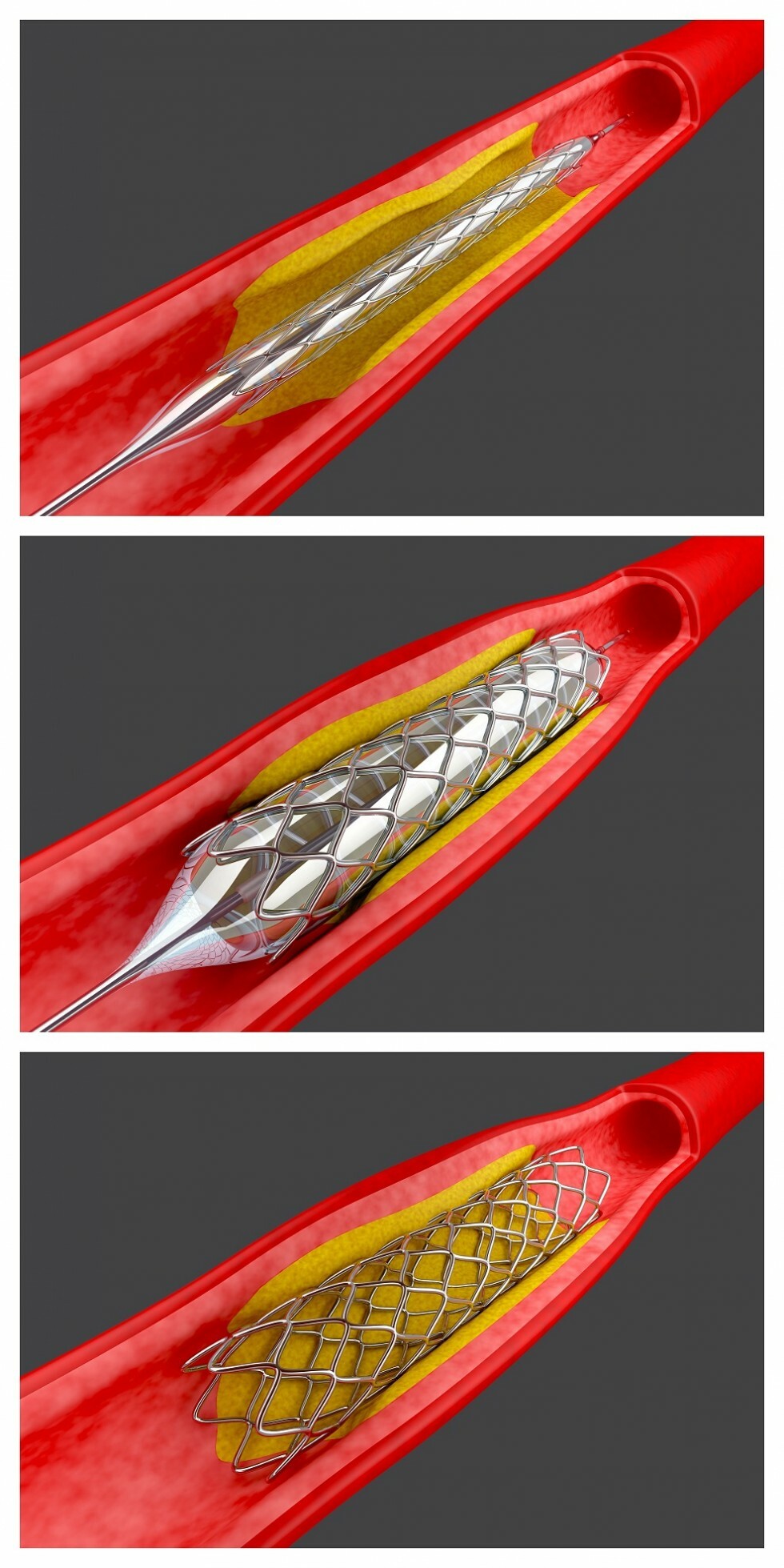
Hepatic Artery Chemoembolization
What is Hepatic Artery Chemoembolization?
Liver cancer may originate in the liver or may spread from another area in the body. Surgery is the best treatment, however up to 80% of liver tumors cannot be surgically removed due to the vascular supply and potential damage that may be caused to the liver. Many liver tumors also do not respond well to traditional chemotherapy.
Your physician will order a CT Scan or MRI to determine the extent of your disease. It is also important to monitor liver function, which is done by a simple blood test. Liver function will be monitored before and after any treatment.
Your liver has two lobes (left and right). Tumors may be present in one or both lobes. If this is the case, each lobe will usually be treated separately to prevent potential damage to the liver.
How does Hepatic Artery Chemoembolization work?
The procedures are performed by an Interventional Radiologist. Interventional radiology is a medical specialty that requires special training. This training includes the use of X-rays and other imaging techniques (radiology) that “see” inside the body without surgery. Interventional Radiologists also undergo extensive training in techniques that treat diseases percutaneously (through the skin) using radiological imaging to guide their procedure.
Prior to the procedure you will not be able to eat or drink for eight hours. You may take your medications with a sip of water. Blood thinning medicine, including aspirin, needs to be stopped at least five days prior to the procedure. You should check with your physician to make sure your medications are safe to take.
An IV will be started in your arm and you will be given several medications including antibiotics and medicine to prevent nausea. During the procedure you will receive medication through your IV to make you sleepy and comfortable. The procedure takes one to two hours to perform.
How is Hepatic Artery Chemoembolization administered?
During the procedure, an angiogram will be performed. A small catheter is placed into the artery in your groin. Small amounts of dye are injected into the catheter. X-ray pictures are taken to identify the branches of the artery supplying blood to the tumor(s). Up to three chemotherapy drugs, mixed together, are then injected into that artery. An oil contrast added to the chemotherapy helps to keep the drugs in contact with the tumor(s). Tiny particles are added to the end of the injection to slow the blood flow to the tumor(s).
The benefits of chemoembolization include:
- The tumor(s) becomes starved of oxygen and nutrients after the blood supply is compromised.
- The drugs are delivered directly to the tumor(s) and are much more concentrated than standard chemotherapy.
- The drugs can affect the tumor(s) for a longer period of time- up to a month.
- There is a decrease in side effects because the chemotherapy does not circulate throughout the body as standard chemotherapy does.
What should I expect after Hepatic Artery Chemoembolization?
Following the procedure, you will be treated with intravenous fluids, pain medication and antibiotics overnight in the hospital. You will need to lie flat for several hours to allow the artery in your groin to seal. You may eat following the procedure.
You will be sent home on antibiotics and medication for pain and nausea if needed. Side effects of the procedure include varying degrees of pain, fever and nausea. These symptoms usually last for several days. You may experience a decrease in appetite. It is important to drink plenty of fluids to prevent dehydration.
Serious complications following chemoembolization are rare. In less than 3% of the procedures, the tumor affected by the procedure may become infected. Severe liver damage, though extremely rare, may also occur.
Chemoembolization will not cure liver cancer. The goal of the treatments is to stop the tumor(s) from growing, reduce tumor size, decrease pain, and preserve liver function.
When should I call my doctor?
Following the procedure, you should call your doctor if you develop:
- Fever greater than 102.0
- Severe pain or nausea
- Bleeding or swelling at the groin site.
A CT scan or MRI will be performed one month after the procedure to determine the treatment effectiveness. Usually two to four treatments are necessary.
Radiofrequency Ablation
What is Radiofrequency Ablation?

Radiofrequency ablation (RFA) is another treatment option for liver tumors. RFA may be performed alone or in combination with surgery or hepatic chemoembolization.
How does Radiofrequency Ablation work?
Radiofrequency ablation begins with the passing of alternating current through a tumor. Heat is applied at the site of the tumor destroying the tumor cells. Several tumors can be treated at one time.
How is Radiofrequency Ablation administered?
After numbing the skin, a tiny probe is placed through the skin in your abdomen into the tumor(s). This is performed with the assistance of ultrasound or CT Scan.
Will I need more than one Radiofrequency Ablation?
Following the procedure, you should call your doctor if you develop:
- Fever greater than 102.0
- Severe pain or nausea
- Bleeding or signs of infection at the puncture site
For more information about this procedure or general information about our interventional radiology practice, please contact one of our clinical coordinators at 513-527-9999.
Renal Artery Stenosis
What is Renal Artery Stenosis (RAS)?

RAS is a condition in which the artery that supplies blood flow to the kidney becomes blocked.
What causes RAS?
Atherosclerosis is the primary cause of RAS(60-70%). Also known as plaque, this is a buildup of cholesterol in the artery. Atherosclerosis is most common in people over the age of 50, and there is a higher incidence in African Americans.
Fibromuscular Dysplasia (FMD) is another cause that accounts for 30-40% of RAS cases. This is a disease in the muscular lining of the artery that causes narrowing of the renal artery. This occurs mostly in younger women. The cause of FMD is unknown. FMD is successfully treated with Renal Artery Angioplasty.
What are the symptoms of RAS?
- High blood pressure that does not respond to blood pressure medication
- Deterioration of kidney function because the kidney is unable to excrete toxins from the body.
What can happen if RAS is not treated?
If the kidney is starved of blood flow, it will be unable to filter waste and toxins from the body. Decrease in blood flow can cause permanent kidney damage that may lead to kidney failure. When the kidney(s) sense a reduction in blood flow, a hormone called renin is secreted that further raises blood pressure. This results in a condition known as renovascular hypertension. The following tests can be used to diagnose renal artery stenosis:
- CTA—Computed Tomography Angiography
- MRA—Magnetic Resonance Angiography
- Angiography
What should I expect before my angiogram?
- Do not eat or drink for 8 hours prior to your procedure.
- Unless you are on a fluid restriction drink plenty of fluids, especially water, the day before your procedure.
- If you are diabetic, your insulin or medication will be adjusted.
- You may be given a medication called Mucomyst to help protect your kidneys from the dye.
- When you arrive at the hospital, blood work will be drawn to check your blood counts and kidney function.
- You will meet the interventional radiologist who will be performing your procedure.
What happens during my angiogram?
You will be placed on an X-ray table and an iodine solution will be applied to your groin area to remove bacteria from the skin. You will be given medication through your vein to make you sleepy. You will be awake but comfortable during the procedure.
You will receive a local anesthetic that will numb the skin at the top of your leg, which may feel like a bee sting. Then a thin catheter will be inserted through the skin into a small opening in your artery in order to see the blood flow to your kidneys. An X-ray dye will be injected to visualize the artery better and determine if a blockage is present. The blood flow to the right and left kidney will be examined during the angiogram.
The angiogram will last approximately 45 minutes.
What is Renal Angioplasty?
If a blockage is found, the interventional radiologist will perform the angioplasty. Interventional radiologists are doctors who have special training to diagnose and treat conditions using tiny, miniaturized tools while watching their progress on X-ray or other imaging equipment.
Another thin catheter will be inserted into the renal artery. This catheter has a balloon on the tip of the catheter. The balloon is inflated and deflated several times causing the plaque to be compressed along the wall of the artery. This opens the artery and restores blood flow to the kidney.
A small metal coil, called a stent, may be placed in the artery to hold the artery open, thus preventing a blockage in the future.
This part of the procedure will last about 30- 45 minutes.
What should I expect after the procedure?
A plug made of collagen is placed into the catheter insertion site to seal the artery. You will not require any sutures. Your body will absorb this over the next few weeks.
After the angiogram you will have to lie flat for a few hours and then you will be discharged. If angioplasty is indicated, you will be kept overnight in the hospital, and then you will be discharged home the following morning.
You should notify your doctor if you experience:
- A lump bigger than the size of a walnut in your groin area
- A fever
- Extreme pain or discomfort in the groin area
- Redness or drainage at the groin site
- If your groin begins to bleed, apply pressure to the area and call 911.
For more information about this procedure or general information about our interventional radiology practice, please contact one of our clinical coordinators at 513-527-9999.
Venous Access
What is a venous access device?
A venous access device is a term commonly used to describe an implantable port. An implantable port is a device that is placed under the skin in either the upper arm or chest. It is used to deliver long-term medications such as chemotherapy into the bloodstream. All ports consist of a small chamber (“the port”) and a catheter. The port has an area of self-sealing silicone rubber in the center called the septum. The catheter is a flexible hollow tube. One end is securely attached to the port, and the other end is placed into a large vein.
How does the interventional radiologist implant the port?
Insertion of an implantable port is a brief procedure that is performed under local anesthesia. Interventional radiologists use ultrasound or contrast-enhanced fluoroscopic guidance techniques that allows accurate visualization of the target vein. The interventional radiologist makes a small incision to create a space or “pocket” for the port under the skin where it will be placed. The port is inserted under the skin and the catheter is placed within a nearby vein. The incision is stitched closed and kept covered with a small dressing until is has completely healed, a process that usually takes a few days. You are sent home within 2 hours following the procedure.
How do I take care of my port?
You will keep the incision clean and dry for 7 days and observe for any signs of infection. It is also necessary to keep the site covered with a small dressing (this will be given to you) for 7 days following implantation. After your incision has healed, there is no special care of the area required. However, you should inspect the skin area around the port on a routine basis. If you observe redness, tenderness, irritation, swelling, or any unusual symptom, you should report this immediately.
Can my port be used immediately after it is inserted?
How long will I have the implantable port in place?
Your port can remain in place as long as your doctor feels you need it. As long as the system is periodically flushed to keep the catheter from becoming blocked, the port can remain under the skin indefinitely.
Sclerotherapy
What is sclerotherapy?

Sclerotherapy is a safe, proven and effective non-surgical procedure used to treat various sizes of veins. Sclerotherapy is a simple technique performed in the interventional radiologist’s office.In addition to offering obvious cosmetic results without scarring, sclerotherapy eliminates the burning, aching and discomfort often caused by varicose veins. With the availability of sclerotherapy, it is no longer necessary to strip varicose veins extensively, a technique resulting in multiple scars and a significant recurrence rate.
Who are the best candidates for sclerotherapy?
Women of any age may be good candidates for sclerotherapy, but most fall between 30 – 60 years old. In some women, spider veins may become noticeable in the teen years. For others, the veins may not become obvious until later in life or after child bearing. These long-term visible varicosities may actually be a sign that there are greater venous insufficiency issues that, if left untreated, could lead to swelling, pain, pigment change, or ultimately ulceration. Spider veins in men aren’t nearly as common as they are in women.
Men who do have spider veins often don’t consider them to be a cosmetic problem because the veins are usually concealed by hair growth on the leg. However, sclerotherapy is just as effective for men.
What is the sclerotherapy procedure like?
Prior to the procedure, you will have an initial consultation to determine if you are eligible for sclerotherapy. This includes an ultrasound of the veins to evaluate the full extent of the problem causing the spider veins. The doctor’s goal is to find the largest vein, which is likely at the root of the problem. This larger vein must be treated before sclerotherapy is performed. If the vein causing the problems is not treated first, other spider veins will appear after the sclerotherapy is complete.
During sclerotherapy, the patient will lie on a table. No sedation is required because there is not a significant amount of discomfort during this procedure. The doctor will make small injection of irritating solution into the vein, which causes the vein to close. The vein then disappears as it is absorbed by the body through the body’s natural healing mechanism.
After each sclerotherapy session, the veins will appear lighter. Two or more sessions are usually required to achieve optimal results. Patients also should be aware that the procedure treats only those veins that are currently visible; it does nothing to permanently alter the venous system or prevent new veins from surfacing in the future.
How long does the sclerotherapy procedure take?
This depends on the number of veins being treated. On average, the total procedure takes about 30 minutes to 1 hour. Each injection is extremely quick, lasting approximately 5 to 10 seconds.
How safe is sclerotherapy?
Complications from sclerotherapy are extremely rare when the procedure is performed by a qualified interventional radiologist. However, it is possible for complications to occur. Risks include the formation of blood clots in the veins, severe inflammation, adverse allergic reactions to the sclerosing solution and skin injury that could leave a small but permanent scar.
Are there any side effects of the sclerotherapy treatment?
A common cosmetic complication is an irregular coloring on the skin – brownish splotches on the affected skin that may take months to fade, sometimes up to a year. Another problem that can occur is fine, reddish blood vessels appearing around the treated area, which would require further injections.
You can reduce the risks associated with treatment by choosing a doctor who has adequate training in sclerotherapy and is well versed in the different types of sclerosing agents available.
How long do the effects of the sclerotherapy treatment last?
The effects of the treatment usually last six weeks for an average case of small vein disease and 8-9 weeks for larger varicose veins. Studies have shown that as many as 50-80% of injected veins may be eliminated with each session of sclerotherapy.
Less than 10% of the people who have sclerotherapy do not respond to the injections at all. In these instances, you should ask your doctor about other options. Although this procedure works for most patients, there are no guarantees for success.
Will I need repeat the sclerotherapy procedure to maintain or improve my look?
The affect of sclerotherapy lasts for approximately two years if the whole spectrum of venous insufficiency is thoroughly reviewed and treated appropriately. After two years, there may be some recurrence, but it usually is never as bad as the initial presentation. The veins that may return also can be treated with sclerotherapy.
Are there any other procedures for the treatment of spider veins?
If sclerotherapy is not successful for your situation, a procedure called stab phlebectomy may be another option. This is involves the use of a special local anesthetic that is injected into the area surrounding your vein. The doctor then removes the entire problem vein through a small incision.
Does my insurance provider cover this procedure?
A number of insurance companies are paying for vein procedures. For more information about this procedure or if you have insurance questions, please contact us at 513-527-9999.
TIPS - Transjugular Intrahepatic Portosystemic Shunt
What is TIPS?
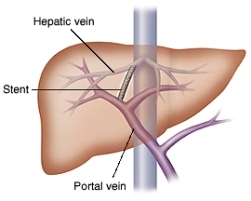
TIPS is a procedure that helps correct blood flow problems in the liver, which is a common side effect of liver disease. The procedure is an alternative to surgery. An interventional radiologist performs the procedure.
What is portal hypertension and what causes it?
TIPScan often help a condition called portal hypertension, which occurs when the normal flow of blood through the blood vessels in the liver is slowed or blocked by scarring or other damage. The scarring or damage is caused by liver diseases, such as hepatitis or cirrhosis.
Several things can happen when the blood vessels are blocked. Sometimes bleeding occurs when the blood tries to find unblocked pathways. In other instances, fluid accumulates in the area around the stomach or in the chest.
How does the TIPS procedure work?
The interventional radiologist makes a tunnel in the liver through which the blocked blood can flow. After the tunnel is made, the doctor inserts a small metal tube (called a shunt or stent) into the tunnel to make sure the tunnel stays open. The interventional radiologist uses X-rays and X-ray dye (also called contrast) to guide the procedure.
What happens before the TIPS procedure?
Patients usually receive medication before the TIPSprocedure to make them very groggy. Sometimes patients are put completely to sleep by an anesthesiologist. In any case, the patient will be given medication to take away pain.
The interventional radiologist performs the entire procedure through an I.V. tube in the neck. If you are not put completely to sleep, the doctor will numb the area before putting in the I.V. tube.
When the procedure is finished, the doctor may leave the I.V. tube in your neck so you can receive other medication through it. Stitches are not necessary when the I.V. tube is removed.
What should I expect after the TIPS procedure?
You will return from the radiology department to your room. The doctor and nurses will tell you when you can eat and how long you will have to stay in bed. Your stomach and/or neck may be sore. There also may be some swelling or bruising in your neck. The soreness and swelling will go away in a few days to a week and generally requires no treatment.
Your TIPS will require periodic check-ups. Your doctor will need to make sure that the TIPS is working well. This is usually done at three, six, or 12 months after the TIPS procedure. Your doctor will tell you the exact schedule you should follow.
What are the benefits of TIPS?
The benefit of TIPS is that your symptoms can be relieved without surgery, and recovery time is less than it would be after surgery.
What are the risks of TIPS?
Any procedure involving blood vessels raises the risk of bleeding. Recent studies indicate that the risk of serious bleeding is about one to two percent.
Some patients get sick from the X-ray dye. This is more likely in patients with diabetes, kidney disease, asthma or a previous allergic reaction to X-ray dye. If you have one of these conditions, tell your interventional radiologist before the procedure begins.
About ten percent of the time, patients become temporarily confused or disoriented as a result of TIPS. This can usually be treated with medication after the TIPS procedure.
Because everyone is different, there may be risks that are not mentioned here. The risks to you will be discussed in more detail by a member of your interventional radiology team.
Treatment of Deep Venous Thrombosis (DVT)
What is Isolated Thrombolysis?
Deep Vein Thrombosis (DVT) is a blood disorder resulting from the formation of a blood clot (thrombus) inside a deep vein of the leg or arm. DVT occurs when the blood clot either partially or completely blocks the flow of blood in the vein. Patient symptoms include pain, swelling, and discoloration.
What are treatment options for DVT?
IV Anti-coagulation Therapy (clot-dissolving drugs or blood thinners), Catheter Directed Thrombosis (using a catheter in the vein to administer anti-coagulation medication), and Catheter Directed Isolated Thrombosis.
What is Isolated Pharmacomechanical Thrombolysis/Thrombectomy?
Utilizing the Trellis® Peripheral Infusion System a catheter with two occluding balloons, drug infusion holes between the balloons, and mechanical drug dispersion capabilities enables physicians to provide focused treatment of thrombus and remove it completely from the blood vessel.
How is Isolated Thrombolysis performed?
The Interventional Radiologists obtains standard venous access by inserting a catheter into the vein. The catheter is guided through the venous system with an external x-ray and advanced through the blood clot. A balloon is then inflated on each side of the clot before the blood thinning medication is administered. Once in place thrombolytic drugs are administered directly to the clot. The rotating wire in the catheter is then activated to help break up the clot. Once the clot is broken up the remaining clot material and thrombolytic drugs are removed through the catheter. The procedure takes approximately 1-2 hours and the patient is relieved of symptoms almost immediately, has a reduced risk of pulmonary embolism, and is not required to stay in the intensive care unit.
What are the benefits of Isolated Thrombolysis?
- Shorter treatment times – a few hours versus a few days.
- The balloons isolate the thrombolytic agent.
- Disperses drug throughout the clot, allowing the drug to act more quickly than catheter directed thrombosis alone.
- The thrombolytic agent is aspirated through the catheter.
- The vein is immediately unblocked and inline flow is restored, which leads to cessation of patient’s symptoms.
Why is DVT so dangerous?
DVT is the main cause of pulmonary embolism. According to the Society of Interventional Radiology, “In the United States alone, 600,000 cases of pulmonary embolism are diagnosed each year. One in every 100 people who develops DVT will die due to pulmonary embolism. PE contributes to 200,000 deaths annually."
What is a Pulmonary Embolism?
Pulmonary embolism is a condition that occurs when a blood clot breaks off and travels through the veins and becomes trapped in the lung, where it blocks the oxygen supply. Most clots originate in the legs but can also come from other parts of the body. Pulmonary Embolism is one of the leading causes of hospital deaths.
What causes DVT?
There are three principal factors that cause DVT. They are reduced blood flow in deep veins (venous stasis), injury to the blood vessel wall, and an increase in activity of clotting substances in the blood (hypercoagulability) .
There are a number of factors that can bring about these conditions and increase the possibility of developing DVT:
- Immobilization, such as lying in bed following surgery
- Having undergone a surgical procedure
- Having been subjected to major trauma
- Increasing age
- Malignancy (cancerous tumor)
- Heart failure
- A previous DVT
- Pregnancy
- The use of oral contraceptives
Uterine Artery Embolization
What are uterine fibroids and what problems do they cause?
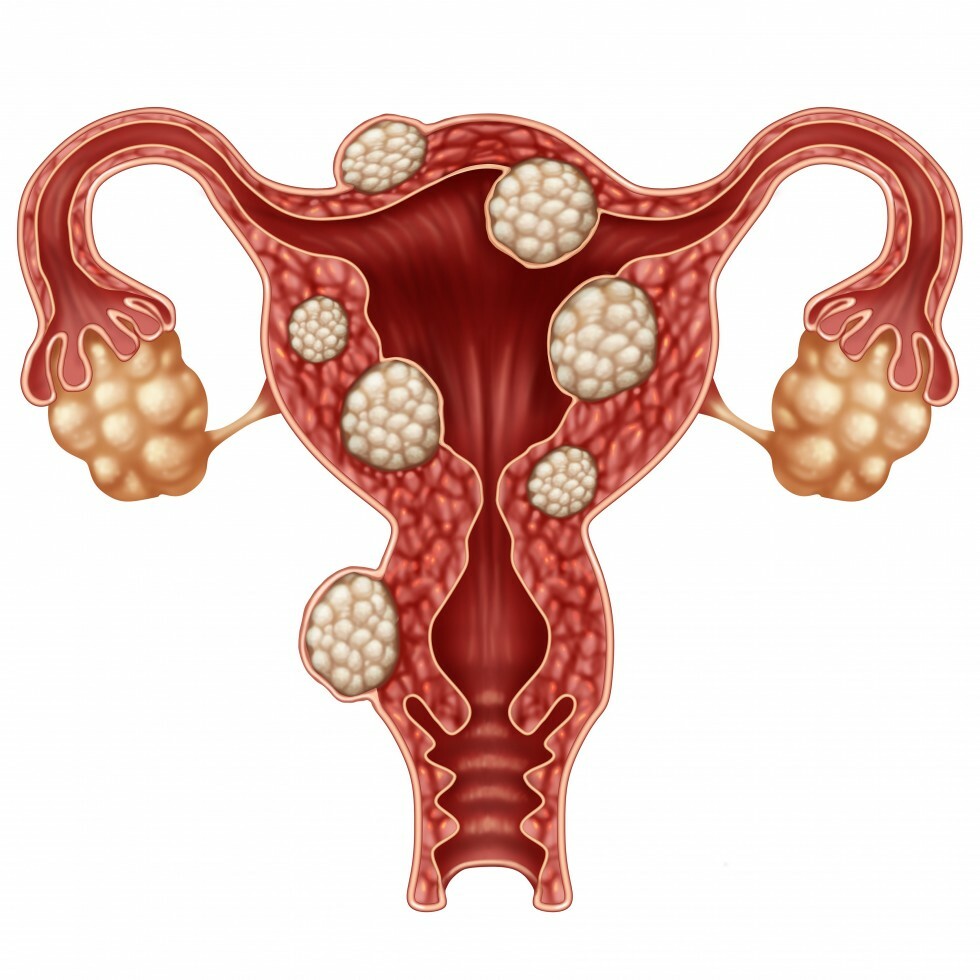
A fibroid is a benign tumor that forms from a single smooth muscle cell that has lost its normal growth control. Fibroids are extremely common and may be found in 20 to 40% of women 35 years of age or older. Fibroids increase in size and frequency with age, but they tend to regress following menopause. Fibroids range in size from very tiny to the size of a cantaloupe or larger. Fibroids can be located in various parts of the uterus, causing different symptoms. Many fibroids do not cause symptoms and no treatment is necessary. However, these non-cancerous growths can cause excessive uterine bleeding, pelvic pain/pressure, urinary problems, backaches, bloating, and cramping.
What is uterine artery embolization (also referred to as uterine fibroid embolization)?
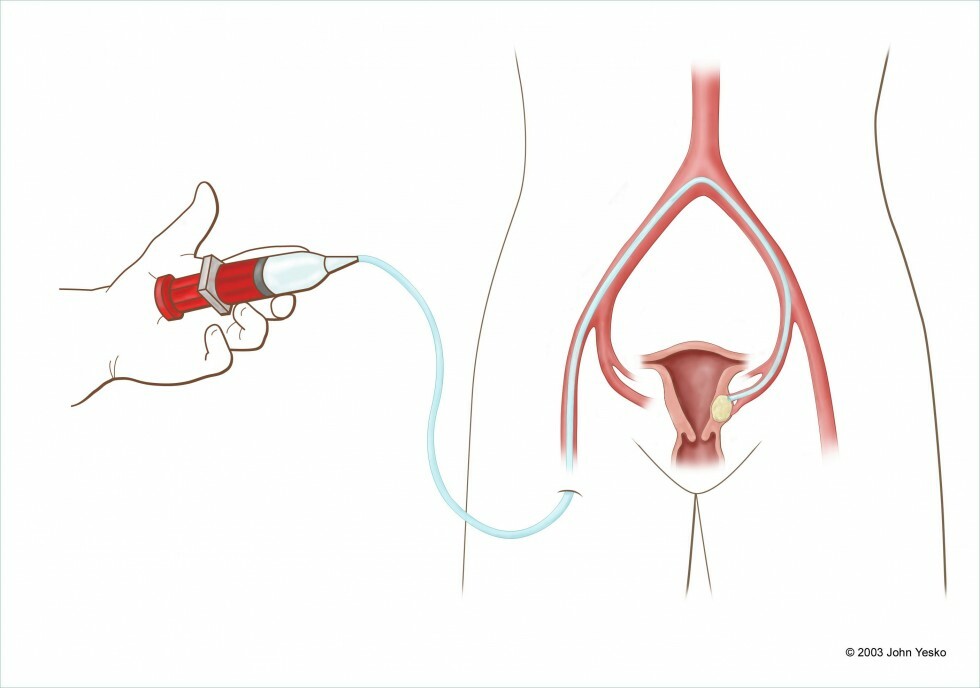
Uterine artery embolization is an established, safe and effective treatment for uterine hemorrhage that accompanies a number of conditions like post-partum bleeding, tumors, arterio-venous malformations, and pre-operatively for decreasing blood loss during surgery. Large groups of patients in France and at UCLA in California have undergone uterine artery embolization for treatment of symptomatic uterine fibroids. The results are extremely encouraging. Uterine artery embolization is a non-surgical procedure for the treatment of symptomatic uterine fibroids. It is a minimally invasive procedure preformed under local anesthesia and sedation. The sedative effects of the medications will make you drowsy. The purpose of uterine artery embolization is to block the blood supply that feeds uterine fibroids, thus starving it of its nutrients. Blocking the blood supply or “embolization” of the uterine artery results in shrinkage of the fibroid growths. During uterine artery embolization, a small catheter is inserted into a blood vessel in your groin and threaded into the arteries to your uterus. Tiny particles pass through the catheter and wedge in the small vessels, blocking the blood flow to the fibroid. In the majority of patients, the fibroid will shrink substantially, resulting in alleviation of symptoms. Fibroid embolization usually requires a hospital stay of one night.
How are uterine fibroids diagnosed?
Fibroids are usually diagnosed during a pelvic exam. Your doctor will conduct a pelvic exam to feel if your uterus is enlarged. An ultrasound or MRI most often confirms the presence of fibroids. Appropriate treatment depends on the size and location of the fibroids, as well as the severity of symptoms.
What options are available to women with symptomatic uterine fibroids?
- Hormonal therapy- shrinks fibroids by inducing chemical menopause
- Hysterectomy- surgical removal of the uterus
- Fibroid embolization- minimally invasive procedure with short recovery period and almost immediate improvement
- Myomectomy- surgical removal of the only the fibroid
How successful is the procedure?
Studies show that 78 to 94% of women who have the procedure experience significant or total relief of symptoms. The procedure has worked even when multiple fibroids are involved. No recurrences have occurred in women who have been followed for up to six years.
Why should I choose uterine artery embolization over another treatment option?
- Non-surgical, minimally invasive procedure
- Shorter recovery time, hospital stay – 24 hours
- Preservation of an organ
- No risks associated with general anesthesia
- Symptomatic improvement within days to few weeks
What should I expect after the procedure?
We recommend that you limit your activity the first 24 hours after returning home. You may make trips to the bathroom and kitchen, but many trips up or down the stairs should be avoided. The following day, you may gradually increase your activity, but you should avoid exercise and heavy lifting greater than 10 lbs. for 1 week. Normal activity is permitted starting 2 days after the procedure. Recovery time varies greatly among the women we have treated. Your activity will be limited by your individual symptoms (i.e. pelvic pain, nausea). We will provide you with medication to make you more comfortable during these times. Some women may develop a low-grade fever. This is related to the destruction of the fibroid and not infection. You will be given anti-inflammatory medicine to reduce inflammation. In addition, your activity may be limited by the medication you will be taking to alleviate these symptoms. Most often, symptoms peak 1-3 days after the procedure and resolve by day 5-6. Most women have been able to return to work within 1 week of the procedure.
Does my insurance provider cover this procedure?
A number of insurance companies are paying for fibroid embolization procedures. For more information about this procedure or if you have insurance questions, please contact us at (513) 527-9999.
Peripheral Arterial Disease/Peripheral Vascular Disease
What is Peripheral Arterial Disease/ Peripheral Vascular Disease?
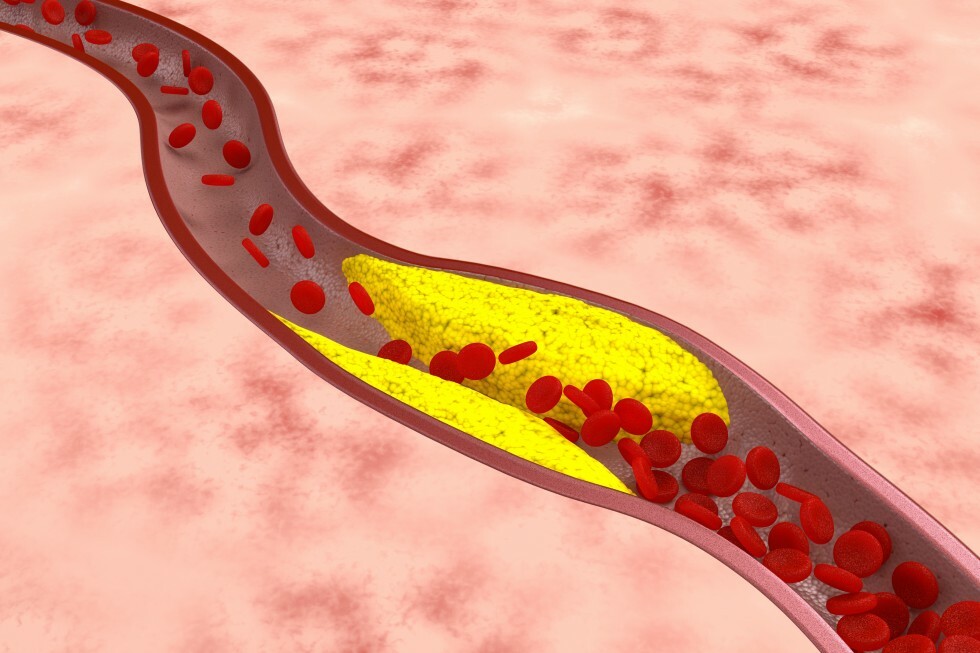
Approximately one million Americans develop symptoms of peripheral vascular disease (PVD) each year. PVD results from the build-up of atherosclerotic plaque in the arteries of the lower extremities causing obstruction of blood flow to the legs and feet. Patients with PVD typically suffer from exercise induced pain the in calf, thigh or buttocks. More advanced cases may present with foot pain at rest, non-healing foot ulcers or wounds, or gangrene.
How is Peripheral Vascular Disease diagnosed?
MR angiography and CT angiography are non-invasive diagnostic tests to evaluate for clogged arteries.
Angiography is an X-ray examination of your arteries. An interventional radiologist places a catheter (a small tube) into one of your arteries and injects contrast into the vessel while taking X-rays of the area. The contrast makes the artery visible on the X-rays. A blockage of an artery can be one of the most common reason for an angiography. An angiogram can tell where the artery is blocked, how severe it is and what is causing it. Common causes could be a blood clot or atherosclerosis (hardening of the arteries). An angiogram has three major steps: insertion of a small catheter (plastic tube) into your body, injection of contrast into an artery while X-ray images are obtained, and removal of the catheter. You will be given a local anesthetic for the catheter insertion and will just feel pressure. Removal of the catheter does not hurt; however, pressure will be placed on the site to stop the artery from bleeding. The angiogram usually takes one to two hours to complete.
What are the risk factors for developing Peripheral Vascualr Disease?
Risk factors include:
- Smoking
- High Blood Pressure
- Diabetes
- High cholesterol
- Obesity
- Sedentary lifestyle
- Family history of vascular disease
What are the treatment options for Peripheral Vascular Disease?
Conservative treatment options, including cessation of tobacco use, exercise programs, and lowering cholesterol levels are the first line of defense against peripheral vascular disease. Many patients with PVD can be treated successfully with minimally invasive techniques such as balloon angioplasty (PTA). Angioplasty involves inflation of a balloon catheter in the diseased artery at the site of blockage. The arterial blockage is stretched open, which establishes a better channel for blood flow. Often a vascular stent is placed concurrently at the site of blockage to mechanically support the diseased artery. The stent decreases the chance that the blood vessel will close up again.
Surgery for peripheral vascular disease is generally reserved for those symptomatic patients who do not respond to conservative treatments and whose vascular anatomy and arterial blockages are not optimal for angioplasty and stent intervention.