FAQs: Neuro Procedures
Epidural Steroid Injection
What causes sciatic pain?
Nerves from the lower limbs (including the sciatic nerve) enter the vertebral column and pierce the dural sac to reach the spinal cord. For various reasons, these nerves can become irritated as they enter the vertebral column and cause pain in the lower limbs. This pain is felt as shooting down the lower limb and is referred to as nerve root pain or, technically, radicular pain (from the Latin radix, a root). The common name for this sort of pain is sciatica.
What is the epidural space in my back?
The spinal cord runs within the bony structure of the vertebral column and is encased by a membranous sac called the dural sac. This sac contains spinal fluid that bathes and nourishes the spinal cord. The epidural space is the space between the outer surface of the dural sac and the bones of the vertebral column.
What is an epidural steroid injection?
The term “epidural steroid injection” (ESI) refers to the injection of a corticosteroid into the epidural space of the vertebral column as a means of treating pain caused by irritation of the spinal nerves.
How does an epidural steroid injection work?
There are two ways, in which an epidural steroid injection is believed to work.
First, some leg pain involves the inflammation of one or more of the nerves, their covering, or their roots, in the back. Thus, the injection of steroids directly into the part of the spinal column called the epidural space is thought to aid in reducing this inflammation.
The other way an ESI works is that the corticosteroid acts like a local anesthetic and block the pain long enough to allow the body to begin the process of repairing itself.
The chief effect of an epidural steroid injection is to reduce pain, but the effect differs from person to person. Most patients will achieve good relief for months after the injection. The goal of your injection is to provide relief so you can begin an appropriate exercise program and return to normal activities/work.
How is an epidural steroid injection administered?
You should not eat or drink 4 hours prior to your procedure.
Please bring your MRI films with you on the day of your procedure.
You will be positioned on a special bed designed for this type of procedure. An IV will be inserted into a vein to administer IV medication, if needed. Local anesthetic will be injected into the skin and underlying tissues to decrease the discomfort of introducing the epidural needle.
Once the local anesthetic is working, the epidural needle is advanced into the epidural space, using the bones as landmarks and a fluoroscopy unit (a type of X-ray) to ensure that the needle is in the right place.
Will I need more than one epidural steroid injection?
Approximately 40% of patients will receive significant pain relief with only one injection. Others require two or three injections to receive maximum symptomatic relief. The injections are usually scheduled at 2-week intervals. Even if epidural steroid injections provide relief, only in exceptional cases would more than three injections be justified within a six month period.
What should I expect after the epidural steroid injection?
You should not drive the day of the procedure. You will experience leg weakness during the first 24 hours following the procedure. To prevent falling, it is important to have someone help you walk. However, you do not need to stay in bed when you get home. In fact, it?s best to walk around if you feel up to it, but you will need assistance during the first 24 hours following the epidural steroid injection. Even if you feel better right away, avoid activities that may strain your back.
After your injection you should feel the same or better for the first 12 hours. The local anesthesia will then wear off and you may experience a return of your pain. The steroid will start working within three days of the injection, with maximal relief at one week. We will contact you one week after the procedure to monitor your pain relief. Keep in mind most patients feel increased pain for the first 24 hours. You should start feeling some pain relief 2-3 days following the injection. This is because the steroid will start working within three days of the injection, with maximal effect by one week. At that time, we will evaluate your pain level to determine the need for another steroid injection.
When should I call my doctor?
Call right away if you notice any of the following symptoms:
- Severe pain or headache
- Fever or chills
- Loss of bladder or bowel control
- Redness or swelling around the injection site
For more information about this procedure or general information about our interventional radiology practice, please contact us at 513-527-9999.
Kyphoplasty
What is kyphoplasty?
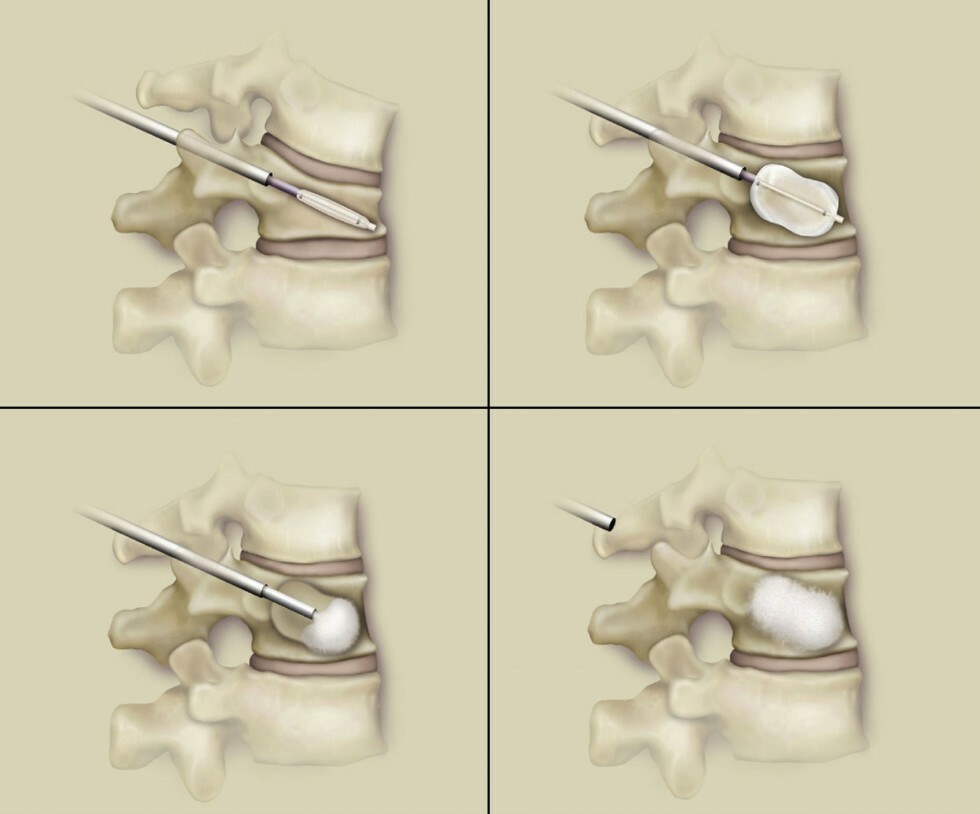
Kyphoplasty is a minimally invasive spinal surgery procedure to correct fractures in vertebra. The kyphoplasty procedure involves the use of a balloon to restore the vertebral body height and shape and is followed by bone cement to strengthen it.
What does kyphoplasty treat?
Kyphoplasty treats osteoporotic fractures in vertebra, which are also referred to as vertebral compression fractures.
What causes vertebral compression fractures?
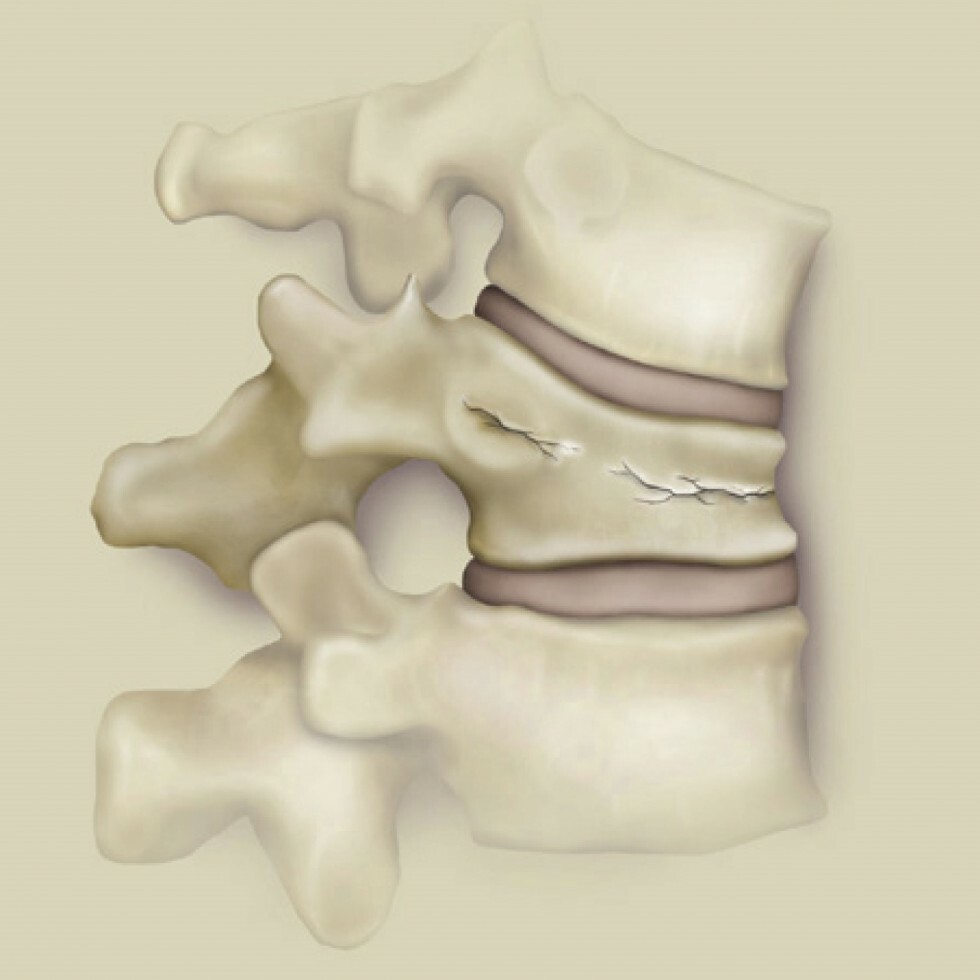
Vertebral compression fractures are most often caused by osteoporosis, which is the loss of calcium from bones resulting in weakened bone structure. Osteoporosis increases the risk of fracture of the vertebral body (the thick block of bone at the front of the vertebrae). Osteoporosis occurs more often in women then men, with women accounting for 80 percent of all osteoporosis cases. Vertebral compression fractures can be also be caused by cancer, arthritis, degenerative disc diseases or trauma to the back, such as a fall or car accident.
What are symptoms of vertebral compression fractures?
A vertebral compression fracture allows the top of the vertebral body to collapse down and produce a “wedged” vertebrae and shortened height. The resulting change in height and spinal alignment can lead to a condition called kyphosis, in which the back begins to round or become hunched.
Symptoms of kyphosis and vertebral compression fractures include:
- Chronic or severe back pain
- Limited function and reduced mobility
- Loss of independence in daily activities
- Decreased lung function
- Difficulty sleeping
- Loss of height
- Decrease appetite
- Depression/anxiety
Who is at risk for vertebral compression fractures?
Those with osteoporosis, cancer, arthritis, degenerative disc diseases or those who have had trauma to the back, such as a fall or car accident are at risk for vertebral compression fractures.
Who is a candidate for kyphoplasty?
Patients experiencing painful symptoms or spinal deformities from recent osteoporotic compression fractures are likely candidates for kyphoplasty. The procedure should be completed within eight weeks of when the fracture occurs for the highest probability of restoring height. Kyphoplasty cannot correct an established deformity of the spine, and some patients with osteoporosis are not candidates for this treatment. You should see your physician for the best treatment option for you.
What should I expect before my kyphoplasty?
Before the treatment, you will have a medical examination and diagnostic studies performed (such as X-rays) to identify the Vertebral compression fractures. The kyphoplasty procedure can be performed while you are asleep (under general anesthesia) or awake (using local anesthesia). Your physician will discuss which option is most appropriate for you.
What happens during my kyphoplasty?
The kyphoplasty begins with a small incision being made in the back through which a narrow tube is placed. The tube creates a path through the back and into the fractured area. Using X-ray images, a special balloon is inserted through the tube and into the vertebrae, then carefully inflated. As the balloon inflates, it elevates the fracture, returning the pieces to a more normal position. After the balloon is removed the cavity is injected with a cement-like material. The cement-like material quickly hardens and stabilizes the bone. The kyphoplasty procedure takes about one hour for each vertebra involved.
What should I expect after my kyphoplasty?
Patients are observed closely in the recovery room immediately following the kyphoplasty procedure. Patients usually leave the hospital the day of the procedure or spend one day in the hospital. Pain relief will be immediate for some patients. In others, elimination or reduction of pain is reported within two days. At home, patients can return to their normal daily activities, although strenuous exertion, such as heavy lifting, should be avoided for at least six weeks. Patients should see their physician to begin a plan to prevent further bone loss.
How successful is kyphoplasty?
Physicians report both short and long term improvements in patients including:
- Significant reduction of back pain
- Improvement of performing daily activities
- Improvement in overall quality of life
- Body height restoration
In a United States study kyphoplasty patients were asked to rate their level of satisfaction with the procedure on a scale from 1-20, where 1 was “completely dissatisfied” and 20 was “completely satisfied.” One week after the procedure the mean score was 17.5 and two years later the median score was 20.
For more information about this procedure or general information about our interventional radiology practice, please contact us by calling 513-527-9999.
Vertebroplasty
What is vertebroplasty?
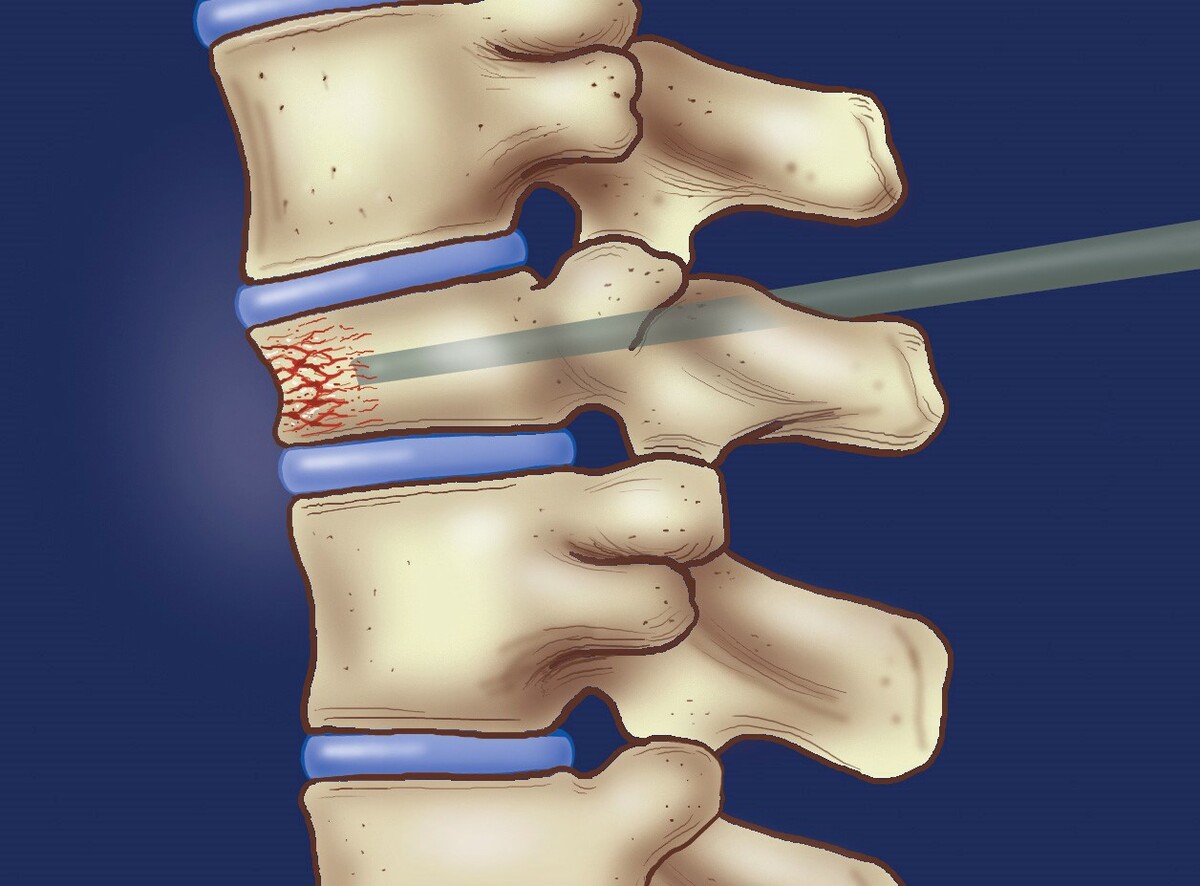
Vertebroplasty is a non-surgical procedure to stabilize broken bones in the spine caused by osteoporosis. In the procedure, a needle about the size of a cocktail straw is inserted through the skin into the crushed vertebrae. Surgical bone cement is injected into the vertebrae to stabilize it. Surgery is not required because the interventional radiologist is able to guide the needle to the right spot using special X-ray equipment. Vertebroplasty takes one or two hours to perform depending on how many bones are treated. The procedure is performed with a local anesthetic that numbs the area to be treated.
Is the procedure safe?
Even though it is a relatively new treatment in the United States, vertebroplasty has been preformed for more than a decade at several centers in France with excellent results. The injection technique has been successfully used for a number of years in the U.S. to treat other conditions in the spine. The bone cement used to stabilize the fractured vertebrae has been shown to be safe through many years of use in joint replacement surgeries and other orthopedic procedures. Vertebroplasty is a very safe procedure with few risks or complications. In many studies, no complications were reported.
Who is a candidate for vertebroplasty?
People who have suffered recent compressing fractures that are causing them moderate to severe back pain are the best candidates for vertebroplasty. In some cases, older fractures may be treated, but the procedure is most successful if it is performed soon after the fracture occurs. The procedure is not used to treat chronic back pain or herniated disks.
How successful is vertebroplasty?
Patients experience immediate pain relief after vertebroplasty. Most report their pain is gone or significantly better within 48 hours. Patients are sent home within 2 hours following the procedure, and can resume their normal daily activities immediately. Studies have shown that from 75 to 90% of people treated with vertebroplasty will have complete or significant reduction in of their pain.
Carotid Artery Stenting
What are the carotid arteries?

Your carotid arteries are the arteries on either side of the neck that supply blood to the head and brain. When plaque builds up inside these artery walls, blockages may form. These blockages restrict the flow of blood and may put you at risk for a stroke. Strokes are the third leading cause of death in the United States, and although strokes have different causes, 20 percent of all strokes are caused by blockages in the carotid arteries.
Am I at risk for a stroke?
You may be at risk for a stroke if you have any of the following:
- Heart disease
- High cholesterol
- High blood pressure
- Atherosclerosis
- Diabetes
You also may be at risk if you have a family history of stroke or if you are:
- Over 65 years old
- African-American
- Overweight
- A smoker
What is carotid arterial stenting?
Carotid arterial stenting is a non-invasive procedure used to open carotid arteries clogged by plaque. During the procedure, doctors use X-rays to guide a catheter in the skin and to the carotid artery. A balloon then is inflated to open up the artery. A small, flexible tube made of plastic or wire, called a stent, then is inserted into the artery to keep the artery open.
Am I a candidate for carotid stenting?
You may be a candidate for carotid arterial stenting if you are at a high risk for surgery or if you have narrow arteries that are difficult to reach and treat with surgery. If you have blockage of a carotid artery and one or more of the risk factors listed below, carotid stenting may be the best treatment option for you.
- Previous carotid surgery
- Previous neck cancer surgery
- Previous neck radiation therapy
- Artery blockage near head or chest
- Complete blockage of the opposite carotid artery
- Severe lung disease
- Severe heart disease